Updated on February 11, 2026
Disclaimers and Disclosures: All information in this article is for informational and educational purposes only and should not be taken as individual medical advice. Additionally, this article contains affiliate links, meaning when you make a purchase, we make a small commission at no additional cost to you. For more information, see our full Disclaimers and Disclosures.
What is a Knee Replacement and Why Would Someone Get One?
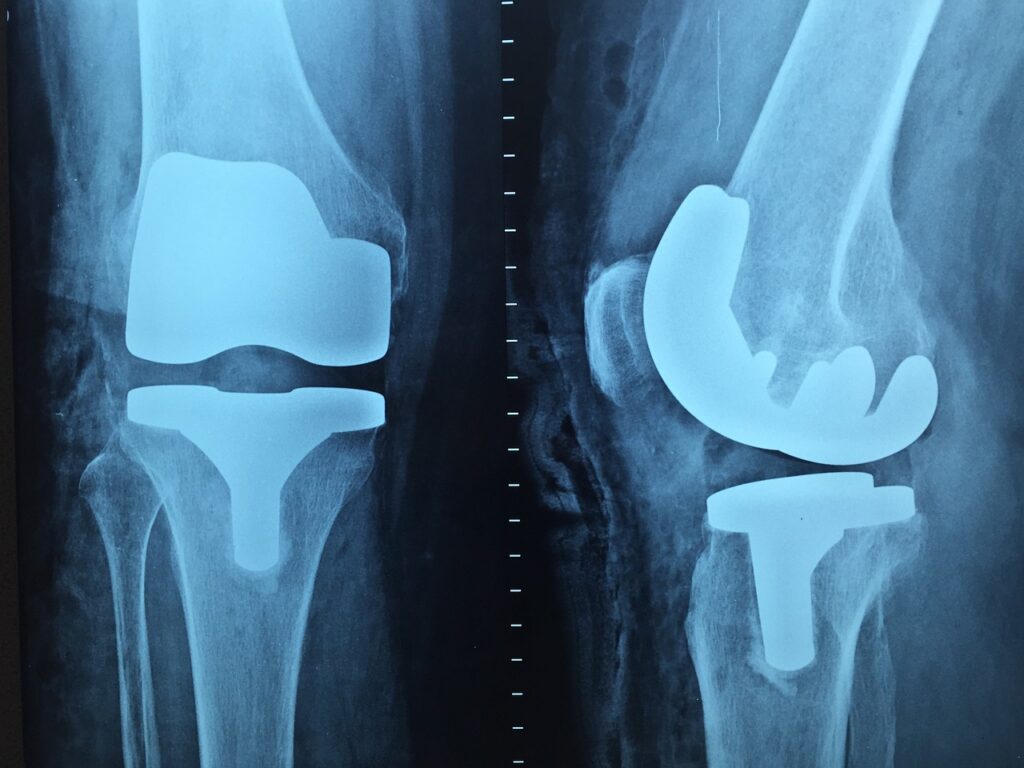
A knee replacement, also known as knee arthroplasty, is when a surgeon will remove damaged or injured parts of the knee joint (bone and cartilage) and insert replacement parts. These replacement parts are made up of metal and plastic components that are applied over the surface ends of the bones which make up the knee joint (femur, tibia and patella).
The purpose of a knee replacement is to improve the function of the knee and reduce pain. As people age, osteoarthritis tends to develop in joints causing pain, stiffness, and swelling which can lead to increased difficulty with activities such as walking, going up/down steps and getting out a chair. By removing the damaged and arthritic sections and resurfacing with new and smooth components, knee function can be restored and the individual can resume normal life activities with less limitation.
What You should do Before Total Knee Replacement (TKR) Surgery.
(1) Weeks before surgery, for best outcomes after surgery, it is recommended for the person to initiate and continue an exercise program. The purpose of the exercises before surgery is to get the leg in the best condition in order for the recovery after surgery to be expedited. Some PT clinics offer a Prehab program for this very reason, to be completed prior to surgery for better outcomes afterwards.
(2) It would also be wise to have an idea of how you will function within your home upon returning from surgery. Activities that may be more difficult to perform initially include going up/down steps, getting up/down from a toilet seat, stepping into/out of a shower among others. Depending on the setup of your home and where your bedroom and bathroom are located, you may need to setup a temporary bed on the floor that has greatest ease of access to the bathroom or kitchen.
(3) Sometimes, a caregiver may be needed initially to assist with cooking, shopping, medication management and even getting dressed with items such as socks, shoes and pants can be difficult initially afterwards. You will also likely need someone to drive to your first follow up appointment with the surgeon as your knee will be stiff, sore, and swollen making driving difficult.
(4) Supplements such as glucosamine, chondroitin sulfate and turmeric can all assist managing knee osteoarthritis. Glucosamine and chondroitin are components that make up the joint cartilage and have anti-inflammatory properties. Although evidence is mixed, it is theorized that they can protect the quality of joint cartilage, slow the process of osteoarthritis from developing and improve function of the joint. Similarly, turmeric is also believed to have anti-inflammatory properties which can assist in joint arthritis, inflammation and swelling.
What to do After Knee Replacement Surgery.
You will likely receive physical therapy in the hospital after your surgery and, even upon waking from anesthesia. You will definitely receive PT the following day and potentially be discharged home that day, pending your progress and symptoms.
Once home, you will possibly receive home health physical therapy. This is when a physical therapist will come to your house to assess your condition and capabilities within the house. The purpose of home health PT is to ensure that you are safe and capable of moving within your own home and to teach you the basic and beginner exercises for which you can complete independently on your own.
Even with these exercises, the primary goal of home health is not to rehab your knee and get you back to 100% but to ensure you are safe and functional at home. For this reason, I do not recommend having home health for >1 week. Too often, patients have had 2-4 weeks of home health therapy thinking they are doing well and begin outpatient PT only to find they have fallen behind and their knee has excessively stiffened. This makes their recovery more uncomfortable and tougher to make gains.
It also complicates the job of the outpatient PT to push them enough to ensure they achieve their rehab goals and outcomes without causing too much pain. By having home health for shorter duration and getting into an outpatient clinic within the first 10 days, you are able to maximize the early period following surgery before the knee stiffens up and becomes even more painful.
I often tell patients that there is a theoretical window for change immediately following surgery. The initial days and weeks after surgery are when the most improvements can be made the quickest. And once that window is closed, gains and progress can still be made but it’s more difficult for everyone involved.
How should I Expect to feel After a Total Knee Replacement?
Following surgery, you can expect to feel stiff, sore and swollen in your knee which can last sometimes weeks to months afterwards. Swelling, in particular, seems to last longer than you would think otherwise. Ways to combat and minimize swelling is to keep moving.
Your body has an internal pump system that works to keep fluid moving and circulating via active movements or muscle contractions. When you walk, your leg muscles have to contract to perform their individual jobs and these cumulative contractions act as a pumping system for the fluid, whether blood in circulation or lymphatic drainage and swelling.
Another secret to help manage the swelling is compression stockings. The key is to get compression stockings that go all the way up to your thighs (called “thigh highs”). Although you may need help donning and doffing, these are a great way to maintain a constant low-level pressure, not only to your knee, but also lower leg, ankle and foot to prevent any pooling or fluid from settling.
Wearing these for most of the day will greatly reduce swelling from accumulating and inhibiting progress. A consistent finding in the clinic is those patients that maintain good compliance with wearing these thigh high stockings typically have much less swelling and progress in their recovery faster.
Notice I did not mention ice or cryotherapy. Although ice can be a great pain management tool, there has been recent findings that suggest ice packs may not inhibit swelling as much as initially assumed. If you are looking for the pain relief that ice can provide following your knee replacement, then you will want ice packs that conform to your knee and are reusable.
What are some Helpful Products after Knee Replacement Surgery?
As mentioned previously, it is important to get up and get moving immediately following surgery (and the weeks afterwards) for many reasons. Initially, most patients will require use of a front wheeled walker (FWW) to help assist them with standing and walking as well as keeping their balance. As expected, your knee is limited with moving and a FWW can be handy for helping assist with balance as well as providing the support needed while you retrain your knee to bend when walking.
The next progression from a FWW is a standard cane (SC). A standard cane will again provide the extra support needed while still practicing a normal gait pattern but is not as cumbersome as a FWW. Some people may be eager to discontinue all assistive devices as fast as possible regardless of what their ambulation quality looks like. I once heard an orthopedic surgeon state that he’d rather have his patients use an assistive device a little bit longer while learning how to properly walk rather than getting rid of the assistive devices too quickly and walking with a significant limp or deviation.
After surgery, your knee will have an approximately 6-8 inch incision along the front. To help with the incision healing in regard to becoming supple and mobile rather than rigid and firm, it is recommended to apply a moisturizing lotion. Once the incision is fully closed and there is no leakage, you can gently massage lotion over the incision. This will also provide some desensitization to the nerve endings that were cut/damaged during the procedure. Some findings suggest coco butter can help the incision blend with the rest of your normal skin tone however there are mixed opinions. For this reason, a Cerave or Aquaphor ointments are sufficient.
Other items that can be helpful in functioning at home include elevated toilet seats, grab handle bars in your shower/tub, shower bench, and long handled shoe horns. These simple gadgets can make a big difference in completing daily activities.
Things Patients Say After Getting Their Knee Replacement
After discussing this topic with several patients, here is a list of several ideas that were mentioned:
One patient was surprised at the difficulty moving and using her leg the days after her surgery. She gave examples of trying to get off a toilet or stepping into a shower/tub were much more challenging than she expected. With the difficulty of moving her leg, she had to compensate by using her other nonsurgical leg, arms and torso when trying to maneuver and manage daily mobility activities. She noted that her whole body was involved rather than only her new knee which she was not expecting.
Another patient described the amount of general fatigue that she experienced was surprising. When it comes to pain and your body recovering from a major surgery, on top of the extra energy expended when trying to perform previously simple activities such as walking, going up/down steps or getting out of a chair, you’ll be using more energy than you’re used to. Thus, you’ll likely be more fatigued than normal.
Based on conversations with patients afterwards, a common theme is the surprise at how much pain they typically experience early on. The main goal of getting a knee replacement in the first place is to lessen the pain in one’s knee and improve function. However, the days and weeks immediately following surgery, pain and hypomobility are typically worse. This is the crucial time when it is most important to stay the course and do the work. The good news is, if patients follow their instructions in their recovery, the pain gradually subsides and overall function gradually improves.
How can I get the best Recovery after a Knee Replacement?
This leads me to the last yet most important aspect of a patient’s recovery after having a knee replacement. And that is to do the work. Among other methods such as soft tissue massage, modalities for pain management, manual stretching and practicing proper walking or going up/down steps, physical therapy will include exercises.
Performing these exercises are one of the most important components of a successful knee replacement recovery. Not only performing the exercises at physical therapy but also at home, every day, multiple times per day. Some of the exercises will cause more pain, however as noted above, the pain will be temporary and the benefits of completing the exercises will lead to long lasting results.
A true successful outcome following a knee replacement surgery (or any orthopedic surgery) comes down to three parties doing their job. The surgeon, the physical therapist and the patient doing the work required afterwards. If any one of these three parties fail in their responsibilities, achieving a good surgery outcome is much more difficult and unlikely.
“There are no secrets to success. It is the result of preparation, hard work, and learning from failure.” -Colin Powell.
Frequently Asked Questions About What to Expect When Getting a Knee Replacement
In the first week, your knee will likely be stiff, swollen, and sore — and that’s normal. You’ll start physical therapy almost immediately (often the same day or next day), focusing on basic movements, walking with an assistive device, and gentle range of motion exercises. Most people also experience fatigue and difficulty performing everyday tasks like getting in and out of bed, stairs, or bathroom fixtures. The goal early on is safety, pain control, and beginning controlled movement.
Pain and swelling are most significant in the first few weeks and gradually improve over the first 3 months. Some swelling can linger up to 6 months or more, especially after activity, but it typically becomes less noticeable over time. Staying active, doing your exercises, and using strategies like elevation and compression can help minimize swelling.
Most patients transition from a walker to a cane and then to independent walking over several weeks. Many people begin walking without assistive devices between 3–6 weeks, but timelines vary based on age, strength, pain levels, and adherence to rehabilitation. Your physical therapist will guide this progression safely.
You’ll usually start physical therapy in the hospital on the day of or day after surgery. If you receive home health therapy, that often continues for a few days before transitioning to outpatient therapy — ideally within the first 10-14 days. Early PT helps restore motion, muscle engagement, and functional mobility.
Most patients can return to normal daily activities like walking around the house, light errands, and basic self‑care within 4–6 weeks, but full recovery — including activities like longer walks, stairs, and community mobility — often takes 3–6 months. High‑impact activities like running usually aren’t recommended long term.
Yes — fatigue is very common after major surgery. Your body is healing while you’re expending extra energy just to do simple movements like sitting, standing, or walking. Proper rest, nutrition, hydration, and pacing yourself with activity can help manage fatigue during recovery.
Movement is one of the most effective ways to reduce swelling since muscle contractions help pump fluid out of the knee joint. Compression stockings (especially thigh‑highs) can also help prevent fluid pooling, and elevation when resting can assist with drainage. While ice is often used for pain relief, its effect on swelling is less clear than previously thought.
Why you can trust Physical Therapy Simplified for what to expect after a knee replacement.
At Physical Therapy Simplified, our mission is to provide an easily accessible and highly reputable source of physical therapy information that anyone can understand, follow, and benefit from. We want you to feel confident that you are getting the best content and information that will help to reduce your pain and restore you to your highest functional potential.
The author of this article, Matthew J. Strano, DPT, is a licensed physical therapist and a Certified Orthopedic Manual Therapist. Additionally, he received his Doctorate in Physical Therapy from Duquesne University. He is an expert physical therapy clinician and specializes in treating orthopedic conditions throughout the body.
Matthew has over ten years of experience in physical therapy and currently works at Vantage Physical Therapy and Rehabilitation. He has treated hundreds of patients after knee replacement surgery and works with individuals to achieve their specific goals and optimal outcomes.




